Oral Diseases and Systemic Infection: Exploring the Surprising Connection
Fact checked
By Lily Duffy, BDS, MRes, MPaed, NHS Leadership Fellow
Last Updated on October 20th, 2023 / Published on September 4, 2023
Your oral health and general well-being are more connected than you may think.1 To achieve good long-term well-being, taking care of your oral health is essential.2
Did you know there is evidence linking gum disease to other chronic diseases?3 It’s associated with diseases such as diabetes, obesity, metabolic syndrome, cardiovascular diseases and stroke.
In this article, you will learn about the diseases that have a proven link to oral health.
Here’s what we know so far about this surprising connection.
Periodontal Disease and its Impact on Systemic Inflammation
Gum disease (also known as periodontal disease) is a process that causes gums to bleed and swell. If left untreated, it progresses to bone destruction and tooth loss.
Gum disease is treatable for most patients, but may be severe and long-lasting if not managed well.
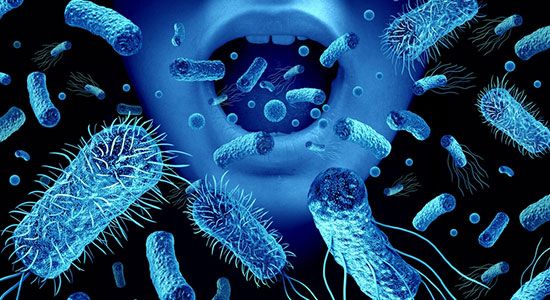
Plaque is a build-up of food and bacteria. This build-up gathers around the teeth and gums. If you don’t remove it by routine teeth brushing, it will cause your gums to swell and bleed. Swelling occurs when your body tries to fight the harmful bacteria, causing what is known as an inflammatory response. This inflammatory response also occurs in other common diseases.4
Systemic Diseases with Connections to Periodontal Disease
Let’s look more into the surprising connection between gum disease and certain conditions.5
Diabetes and Periodontal Health: A Bidirectional Relationship
In diabetes, your body can’t regulate the amount of sugar in your bloodstream. This causes high blood sugar and the same type of inflammatory process observed in gum disease.6
Researchers have found that diabetic patients with gum disease have more difficulties managing their blood sugar than those without gum disease.6 They believe that inflammation caused by gum disease within the body contributes to the worsening of blood sugar control.
The term ‘bidirectional’ describes this relationship because gum disease intensifies the effects of diabetes, and diabetes exacerbates the effects of gum disease.6 This highlights the importance of managing both conditions together to achieve optimal health and general well-being.
Cardiovascular Health and Oral Hygiene: An Intriguing Nexus
The cardiovascular system is the part of the body that controls the heart and blood vessels. As you may imagine, this finely tuned system is very sensitive to inflammation.
Oral inflammation can trigger an inflammatory process throughout the body, with the heart being at the center.7
How Does Oral Bacteria Reach the Heart?
Harmful bacteria can come from sources such as gum disease, tooth decay, and poor oral hygiene. This bacteria can then enter the bloodstream and make its way to the heart and surrounding blood vessels.7
Bacteria can become dislodged from the mouth and enter the bloodstream. This could be due to routine habits such as tooth brushing and eating. More invasive procedures such as dental extractions or root canal fillings can also trigger this process.8
Endocarditis: The Heart’s Response to Oral Bacterial Invasion
If bacteria reach your heart, they may attach to delicate structures such as the heart valves. Heart valves play a crucial role in regulating blood flow through the heart. If harmful bacteria damage these valves, their ability to function becomes compromised.8
This in turn can increase the risk of cardiovascular events, such as endocarditis, blood clots, and stroke.
Respiratory Diseases and Oral Health: Unraveling the Connection
Like the cardiovascular system, the respiratory system is a series of related structures – the nose, windpipe, and lungs.
These structures link to the mouth and bacteria within it. Bacteria present in the mouth caused by gum disease can reach the lungs through normal functions such as breathing and swallowing.9 This increases the risk of breathing difficulties and infection.
Rheumatoid Arthritis and Gum Disease
Arthritis is inflammation in joints and tendons. It can affect most areas of the body but often starts in the joints of the hands and neck.
Research has found that the harmful bacteria responsible for gum disease also exist in the joints of those with arthritis. This finding suggests that the processes that cause gum disease may be a trigger for arthritis.10
This supports the concept that improved management of gum disease can lead to improved management of arthritis, and vice versa. New research suggests that effective management of one condition may lead to improvements in the other.10
Pregnancy and Oral Health: Impacts on Maternal and Fetal Well-being
Common sense tells us that good oral health is a good idea for an expectant mother, as is good health and well-being. Yet, research now indicates that good oral health in the mother is as important to the unborn baby as well.
The placenta is the protective barrier that develops alongside a growing fetus. Its function is to prevent harmful bacteria and other toxins passing through the mother’s bloodstream to the baby. Yet, research has found that bacteria present in the mother due to gum disease can pass through this protective barrier, directly to the fetus. This results in health issues during birth such as premature birth and low birth weight.11
The Role of Oral Health Interventions in Managing Systemic Diseases
As a reader, you are not alone in finding this information surprising! The eye-opening link between gum disease and bodily diseases is remarkable, and still in the early stages of research.
These findings should serve as a reminder that routine dental check-ups are crucial, not only to your oral health but to your well-being too! You should aim to see the dentist at least twice a year for check-ups, and always return for any follow-up treatment.12
Holistic Approach to Healthcare: Addressing Oral and Systemic Health Together
As the saying goes, with knowledge comes power! Understanding the effect of oral health on systemic conditions allows dental and medical professionals to work together, providing a united approach to healthcare.13 Regular and routine care from both professions should treat you holistically. This means they should treat you as a whole person, taking into account all areas of the body, not just the mouth or a single structure such as the heart.
Takeaway
The conclusion is clear – neglecting your oral health can have consequences that reach further than the oral environment. Inflammation and harmful oral bacteria that cause gum disease are found in other bodily diseases like heart disease, diabetes, and arthritis. Evidence links these to gum disease, and shows that improving gum disease can reduce symptoms of the related diseases.
Live a healthy and happy life by prioritizing good oral hygiene practices and routine dental care, free from the potential systemic complications that might arise from oral diseases.
References
- Zemedikun DT, Chandan JS, Raindi D, et al. Burden of chronic diseases associated with periodontal diseases: a retrospective cohort study using UK primary care data. BMJ Open 2021;11:e048296.
- Martínez-García M, Hernández-Lemus E. Periodontal Inflammation and Systemic Diseases: An Overview. Front Physiol. 2021;12:709438. Published 2021 Oct 27.
- Janakiram, C, Dye, BA. A public health approach for prevention of periodontal disease. Periodontol 2000. 2020; 84: 202–214.
- Kane SF. The effects of oral health on systemic health. General Dent. 2017;65(6):30–4.
- Kim, J., Amar, S. Periodontal disease and systemic conditions: a bidirectional relationship. Odontology 94, 10–21 (2006).
- Păunică I, Giurgiu M, Dumitriu AS, Păunică S, Pantea Stoian AM, Martu M-A, Serafinceanu C. The Bidirectional Relationship between Periodontal Disease and Diabetes Mellitus—A Review. Diagnostics.
- Sanz M, Marco Del Castillo A, Jepsen S, et al. Periodontitis and cardiovascular diseases: Consensus report. J Clin Periodontol. 2020;47(3):268-288.
- Gomes, B.P.F.A., Berber, V.B., Chiarelli-Neto, V.M. et al. Microbiota present in combined endodontic-periodontal diseases and its risks for endocarditis. Clin Oral Invest 27, 4757–4771 (2023).
- Muthu, J., Muthanandam, S. Periodontitis and Respiratory Diseases: What Does the Recent Evidence Point to?. Curr Oral Health Rep 5, 63–69 (2018).
- Zhain Mustufvi and others, Does periodontal treatment improve rheumatoid arthritis disease activity? A systematic review, Rheumatology Advances in Practice, Volume 6, Issue 2, 2022.
- Butera A, Maiorani C, Morandini A, Trombini J, Simonini M, Ogliari C, Scribante A. Periodontitis in Pregnant Women: A Possible Link to Adverse Pregnancy Outcomes. Healthcare. 2023; 11(10):1372.
- Lang, NP, Bartold, PM. Periodontal health. J Periodontol. 2018; 89(Suppl 1): S9–S16.
- Periodontists and family doctors must collaborate to treat their patients’ overall health. BDJ Team 10, 4 (2023).